Facial Paralysis: Causes, Symptoms, and Underlying Conditions Explained
Facial paralysis is a condition where you lose the ability to move some or all of the muscles on one or both sides of your face due to nerve damage or dysfunction. While it can result from various conditions ranging from viral infections like Bell’s palsy to more serious issues such as strokes or tumors, most cases are temporary and treatable when diagnosed early. Understanding the warning signs and underlying causes is crucial for prompt medical intervention and better outcomes.
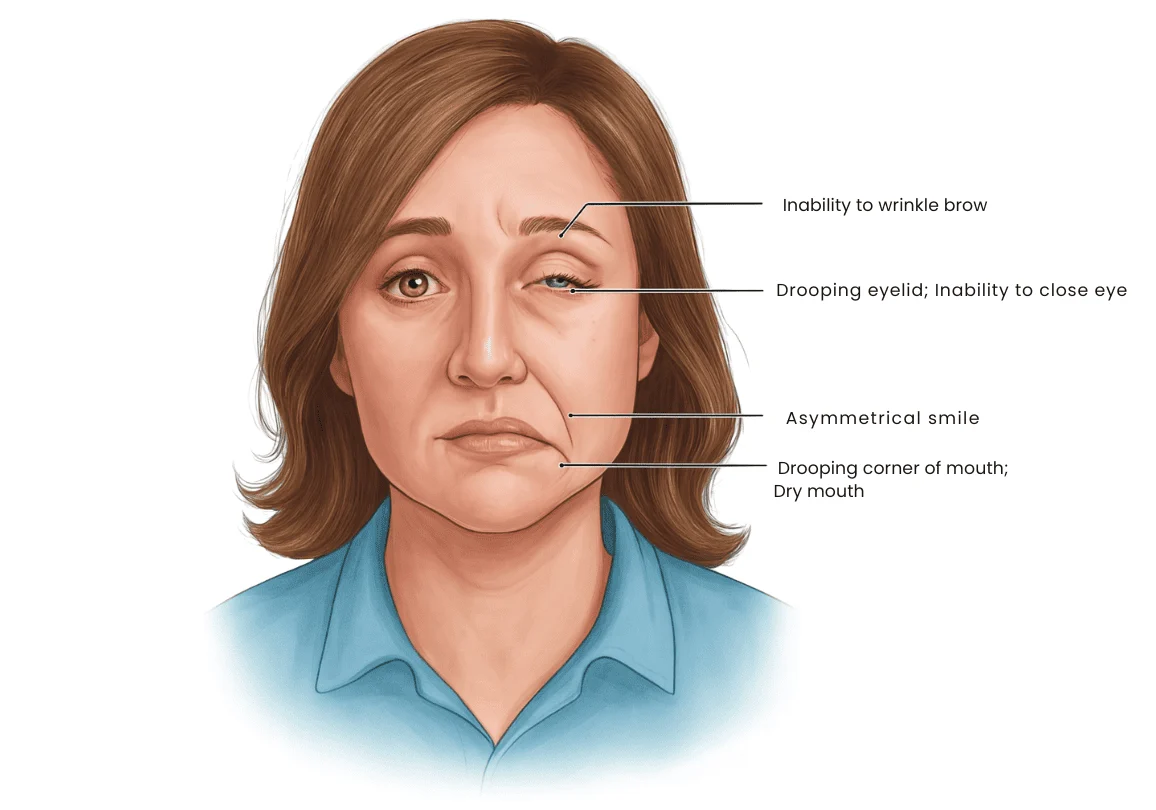
If you’ve ever woken up to find one side of your face drooping, struggled to close an eye completely, or noticed difficulty smiling evenly, you’ve experienced symptoms that warrant immediate medical attention.
What Is Facial Paralysis?
Facial paralysis occurs when the facial nerve (the seventh cranial nerve) becomes damaged, compressed, or inflamed, resulting in weakness or complete loss of movement in the facial muscles. This nerve controls most of the muscles responsible for facial expressions, tear production, and even some aspects of taste and hearing.
The condition can affect people of all ages, though certain causes are more common in specific age groups. The severity can range from mild weakness to complete paralysis, and it may be temporary or permanent depending on the underlying cause.
Common Facial Paralysis Causes
Understanding what causes facial paralysis is essential for proper diagnosis and treatment. The causes vary widely, from relatively benign viral infections to serious medical emergencies.
Bell’s Palsy
Bell’s palsy is the most common cause of sudden facial nerve paralysis, accounting for approximately 60-75% of cases. While the exact mechanism isn’t fully understood, researchers believe viral infections—particularly herpes simplex virus—trigger inflammation that compresses the facial nerve within its bony canal.
This condition typically develops rapidly over 48 hours and can affect anyone, though it’s slightly more common in pregnant women and people with diabetes.
Stroke-Related Facial Paralysis
A stroke represents a medical emergency and is among the most serious facial paralysis causes in adults. Unlike Bell’s palsy, which affects the entire side of the face, stroke-related facial weakness typically spares the forehead muscles because they receive nerve signals from both sides of the brain.
Facial paralysis stroke symptoms include:
- Sudden weakness affecting only the lower face
- Difficulty speaking or understanding speech
- Severe headache with no known cause
- Vision problems in one or both eyes
- Dizziness or loss of balance
- Weakness or numbness on one side of the body
Tumors and Facial Nerve Compression
A tumor causing facial paralysis is less common but requires serious medical attention. Both benign and malignant tumors can compress or invade the facial nerve pathway, leading to progressive weakness.
Acoustic neuromas (benign tumors of the hearing and balance nerve) are the most common benign tumors affecting facial nerve function. These typically cause gradual onset of symptoms including hearing loss, tinnitus, and eventually facial weakness.
Malignant tumors such as parotid gland cancers, temporal bone cancers, or metastatic disease can also affect the facial nerve and usually present with more rapid progression.
Infections and Inflammatory Conditions
Several infections can damage the facial nerve:
- Ramsay Hunt syndrome: Caused by varicella-zoster virus (the same virus that causes chickenpox and shingles), this condition causes facial paralysis along with a painful rash in or around the ear
- Lyme disease: This tick-borne bacterial infection can cause facial nerve inflammation, sometimes affecting both sides of the face
- Middle ear infections: Severe ear infections can spread to the facial nerve
- Viral infections: Various viruses including herpes simplex, Epstein-Barr, and cytomegalovirus have been associated with facial nerve damage
Trauma and Injury
Physical trauma represents another significant cause:
- Skull fractures, particularly those affecting the temporal bone
- Facial injuries from accidents
- Surgical complications during procedures near the facial nerve
- Birth trauma in newborns
Medical Conditions and Systemic Diseases
Can diabetes cause facial paralysis? Yes, diabetes increases the risk of Bell’s palsy by approximately 29% compared to non-diabetics. The exact mechanism involves damage to small blood vessels that supply the facial nerve, similar to other diabetic neuropathies.
Other systemic conditions include:
- Multiple sclerosis
- Sarcoidosis
- Guillain-Barré syndrome
- Autoimmune disorders affecting nerves
Stress and Lifestyle Factors
While facial paralysis caused by stress isn’t a direct cause-and-effect relationship, chronic stress may contribute to conditions like Bell’s palsy. Stress weakens the immune system, potentially allowing dormant viruses to reactivate and trigger nerve inflammation.
Research suggests that physical or emotional stress in the weeks preceding symptom onset may be a contributing factor in some cases of Bell’s palsy.
Recognizing Facial Paralysis Symptoms
Early recognition of facial paralysis symptoms is crucial for timely treatment and better outcomes. The symptoms can vary depending on the severity and underlying cause.
Complete vs. Partial Facial Weakness
Partial facial paralysis may produce milder symptoms than complete paralysis. Partial weakness might manifest as:
- Slight drooping of one corner of the mouth
- Difficulty with subtle expressions
- Mild asymmetry that becomes more noticeable when smiling or talking
- Reduced tear production in one eye
Complete paralysis results in total loss of movement on the affected side.
Key Warning Signs
Facial nerve paralysis symptoms typically include:
- Sudden or gradual facial drooping: One side of your face appears to droop or feel heavy
- Difficulty closing one eye: This can lead to eye dryness, irritation, and potential damage
- Loss of facial expressions: Inability to smile, frown, or raise eyebrows on the affected side
- Drooling: Liquid may leak from one side of the mouth
- Speech difficulties: Slurred or unclear speech due to mouth muscle weakness
- Changes in taste: Metallic or altered taste sensations on the front portion of the tongue
- Increased sensitivity to sound: Sounds may seem abnormally loud in one ear
- Pain around the jaw or behind the ear: Particularly common in Bell’s palsy and Ramsay Hunt syndrome
- Difficulty eating and drinking: Food may collect in one cheek; drinking becomes challenging
When Facial Paralysis Indicates a Stroke
Distinguishing between Bell’s palsy and stroke is critical. Remember the acronym F.A.S.T.:
- Face: Ask the person to smile. Does one side droop?
- Arms: Ask them to raise both arms. Does one drift downward?
- Speech: Ask them to repeat a simple phrase. Is speech slurred or strange?
- Time: If you observe any of these signs, call emergency services immediately
Diagnosis and Medical Evaluation
When you present with facial weakness, your healthcare provider will conduct a thorough evaluation to determine the underlying cause.
Physical Examination
Your doctor will assess:
- The degree and pattern of facial weakness
- Your ability to perform specific facial movements
- Other cranial nerve functions
- Overall neurological status
Diagnostic Tests
Depending on your presentation, tests may include:
- Blood tests: To check for diabetes, Lyme disease, or other infections
- Imaging studies: MRI or CT scans to rule out tumors, stroke, or structural abnormalities
- Electromyography (EMG): Measures electrical activity in muscles and can assess nerve damage severity
- Hearing tests: Especially if acoustic neuroma is suspected
Treatment Approaches
Treatment for facial nerve paralysis depends entirely on the underlying cause and should begin as soon as possible.
Medical Treatments
- Corticosteroids: Reduce inflammation and swelling around the facial nerve, particularly effective in Bell’s palsy when started within 72 hours
- Antiviral medications: May be prescribed alongside steroids for Bell’s palsy or when viral causes are suspected
- Antibiotics: For bacterial infections like Lyme disease
- Eye protection: Artificial tears, eye patches, or surgical procedures to protect the cornea when you cannot close your eye properly
Surgical Interventions
Surgery may be necessary for:
- Tumor removal: When a tumor causing facial paralysis is identified
- Facial nerve decompression in certain cases
- Reconstructive procedures for long-term paralysis
Rehabilitation and Physical Therapy
Facial exercises and physical therapy can help:
- Maintain muscle tone
- Improve coordination
- Prevent permanent contractures
- Speed recovery in conditions like Bell’s palsy
Prognosis and Recovery
The outlook for facial paralysis varies widely:
- Bell’s palsy: Approximately 70% of patients recover completely without treatment, and up to 85% recover with corticosteroid treatment within 3-6 months
- Stroke-related paralysis: Recovery depends on stroke severity and rehabilitation efforts
- Tumor-related cases: Prognosis depends on tumor type, location, and whether complete removal is possible
- Infection-related paralysis: Usually resolves with appropriate antimicrobial treatment
Key Takeaways
- Facial paralysis involves loss of movement in facial muscles due to nerve damage, with causes ranging from viral infections to serious conditions like stroke or tumors
- Bell’s palsy is the most common cause, typically resolving within months, while stroke-related facial weakness requires immediate emergency care
- Recognizing facial paralysis symptoms early—including facial drooping, inability to close an eye, and speech difficulties—is crucial for prompt treatment
- Underlying conditions such as diabetes, tumors, infections, and trauma can all contribute to facial nerve paralysis
- Treatment varies by cause but may include corticosteroids, antivirals, antibiotics, eye protection, or surgery
- Early medical evaluation and intervention significantly improve outcomes for most types of facial paralysis
Frequently Asked Questions
Q: Can facial paralysis go away on its own without treatment?
A: It depends on the cause. Bell’s palsy often resolves spontaneously in about 70% of cases within several months, though treatment with corticosteroids significantly improves recovery rates. However, other causes like tumors, stroke, or severe infections require specific medical interventions and will not resolve without proper treatment. Never assume facial paralysis will resolve on its own—always seek medical evaluation to identify the underlying cause.
Q: Is facial paralysis contagious or hereditary?
A: Facial paralysis itself is not contagious or directly hereditary. However, some underlying causes can be infectious (like Lyme disease transmitted through tick bites, though not person-to-person) or have genetic components (such as predisposition to certain autoimmune conditions). Bell’s palsy shows some familial clustering, suggesting possible genetic susceptibility, but there’s no specific “facial paralysis gene” that parents pass to children.
Q: How long does it take to recover from facial paralysis, and will my face return to normal?
A: Recovery time varies dramatically based on the cause and severity. Bell’s palsy patients typically see improvement within 2-3 weeks and complete or near-complete recovery within 3-6 months. Mild cases may resolve in weeks, while severe nerve damage might take a year or longer. Approximately 15-20% of people experience some permanent residual weakness. Factors affecting recovery include age, severity of initial paralysis, presence of complete versus partial paralysis, and how quickly treatment begins.
Q: What’s the difference between facial paralysis affecting one side versus both sides?
A: Unilateral (one-sided) facial paralysis is far more common and typically suggests localized nerve damage from conditions like Bell’s palsy, stroke, or tumors. Bilateral (both-sided) facial paralysis is rare but more concerning, often indicating systemic conditions like Guillain-Barré syndrome, Lyme disease, or sarcoidosis. Bilateral facial weakness requires urgent medical evaluation as it may suggest a more serious underlying condition affecting the entire nervous system.
Q: Are there any permanent complications from facial paralysis even after recovery?
A: Yes, some people experience long-term complications even after muscle function returns. These include synkinesis (involuntary movements, such as the eye closing when smiling), crocodile tear syndrome (tearing while eating), facial contractures or tightness, chronic facial pain or numbness, and persistent changes in taste or hearing. Corneal damage from inadequate eye closure during the paralysis phase can also cause permanent vision problems. Early treatment and proper eye protection during the acute phase help minimize these complications.
 +919325609388
+919325609388
 +919325609388
+919325609388
Leave a Reply